TMJ and TMD Symptoms and Treatment Overview
Do you ever experience a clicking or popping sound when opening or closing your mouth? Have you been suffering from headaches or migraines and no one seems to be able to help you? Have you been taking pain medicine for years and would like to get off of it? Do you feel any clogging or congestion in one or both of your ears? These are just a few of many symptoms that might be associated with TMD, or Temporomandibular Dysfunction, a common condition affecting the jaw joint or Temporomandibular Joint (TMJ).
TMJ dysfunction, often referred to as TMD, is a disharmony between the way the jaw joint works in an unstrained position and the way the teeth and bite work during those movements. Possible causes of this disharmony include tooth loss, accidents (like whiplash), mal-positioned and/or underdeveloped cranial or jawbones, and perhaps habits like clenching or teeth grinding. Many people go through life suffering from headaches and a variety of facial and neck pains without knowing the ultimate cause, which in many cases is TMJ disorder.
Define TMJ and TMD
TMJ or The Temporomandibular Joint
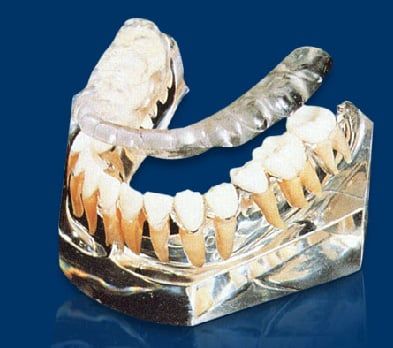
They are the two joints which connect the lower jaw to the temporal bone at the side of the head. If you place your fingers just in front of your ears and open your mouth, you can feel the joint on each side of the head. Because these joints are flexible, the jaw can move smoothly up and down and side to side, enabling us to talk, chew and yawn. When the TMJ is not functioning normally and it is not within its physiological limits, it creates a condition called TMD, or Temporomandibular Dysfunction.
TMD is a group of conditions resulting from not having a normal function or "comfortable" positioning of the TMJ, and will present as a cycle of pain, muscle spasms and jaw problems. When teeth are missing, out of alignment, crowded or misshaped, chewing and biting cannot be achieved in a balanced way, so the TMJ and the muscles of chewing try to compensate for this unbalanced movement which results in symptoms that will confirm the presence of TMD.
Temporomandibular Joint Disorder (TMD) is not just a disorder, but a group of conditions, often painful, that affect the jaw joint or Temporomandibular Joint (TMJ) and the muscles that control chewing.
TMD falls into three main categories:
- Myofascial pain, the most common form of TMD, which is discomfort or pain in the muscles that control jaw functions and the neck and shoulder muscles.
- Internal derangement of the joint meaning a dislocated or displaced disc or injury to the condyle (the rounded part at the end of the jaw bone).
- Degenerative joint disease such as Osteoarthritis or Rheumatoid Arthritis in the jaw joint. Causes of TMJ/TMD
There are many causes for TMD such as:
- Unbalanced occlusion or "Bad Bite"
- Stress (emotional or work/school related)
- Injury or trauma (this could have been an injury as obvious as a blow to the jaw with a fist or something as subtle as a whiplash injury with direct trauma to the head or jaw.
- Teeth grinding or Bruxism
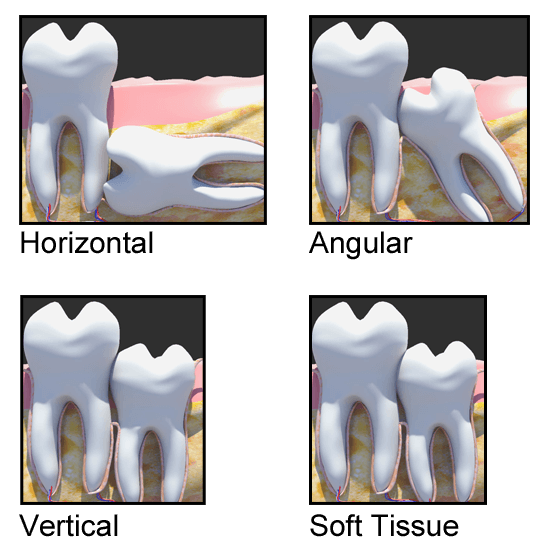
A "Bad Bite" could be caused by any of the following:
- Missing teeth
- Crowded or "crooked" teeth
- Worn down teeth
- Old crowns and bridges
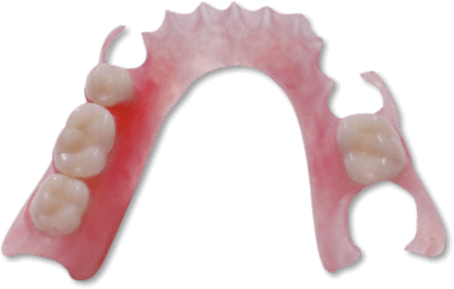
- Unbalanced dentures
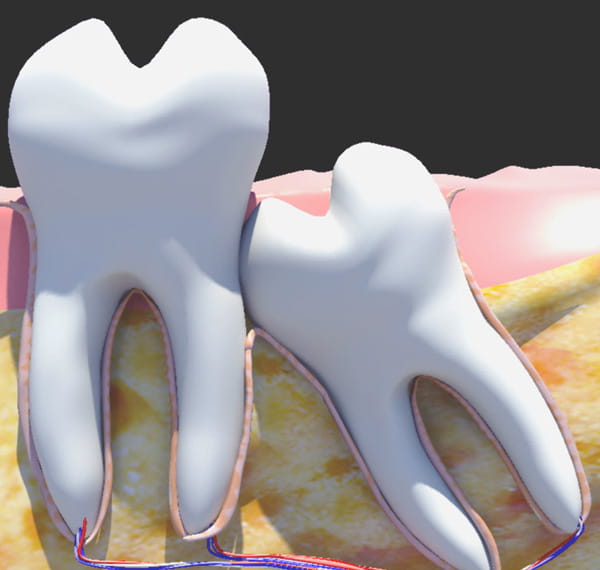
When teeth are missing, or out of alignment, it causes the jaw to shift positions and the muscles to work harder to chew, swallow, bite...etc and eventually will cause: muscle spasms, tension and pain.
Muscle tension and misplaced TMJ could cause the TMJ disc to be pulled out of place which will result in pain, clicking and popping in the TMJ.
If the disc is displaced for a long time, the bones will start rubbing against each other and some damage will happen to the bone, this is called Osteoorthrosis.
If there is inflammation in other joints or bones of the body, it is called Osteoarthritis (Arthritis) which may involve the jaw bone and the TMJ. Some damage to the bone may be evident on the x-rays.
TMD Symptoms
- Headaches, Migraines or tension headaches
- Worn or loose teeth
- Painful muscles in the neck and shoulders (muscle spasms)
- Pain behind the eyes.
- Clicking and popping of the jaw joint (TMJ)
- Locked jaw or restriction in opening or closing the mouth
- Earaches or a clogging feeling in the ears
- Tingling or numbness in the hands and the fingertips
TMJ Diagnosis
While recognizing TMJ problems is within the ability of most physicians and dentists, not all practitioners are qualified to diagnose it properly and treat it right. It is imperative that a trained practitioner in Craniofacial pain or Neuromuscular Dentistry give the final and definitive diagnosis, and suggest the most suitable treatment plan.
There is a lot of skepticism about TMJ treatment in the medical society, and that is simply due to the fact that physicians didn't receive the dental training and didn't acquire the knowledge required for such complicated diagnosis and treatment. Furthermore, many dentists rush into treating TMJ thinking that they can cure these problems, only to find that they lack the skill and experience to get the job done.
We have training and experience in the treatment of these problems with outstanding success rates. With highly advanced equipment and a high level of knowledge, we address your concerns and provide the best diagnosis for the optimal treatment.
Undiagnosed TMJ/TMD
Many patients who suffer from TMD symptoms were never told that it is related to their TMJ problem and were not aware that treating their TMJ could easily relieve their suffering. To explain this further...
Headaches and Migraines
If you suffer from headaches or migraines, TMJ dysfunction, could be the major and most likely cause of your suffering. Your doctors, including neurologists, have simply not received the dental training required to relate your migraine or headache pain to your TMJ problems. Once you rule out any brain tumors or aneurysms, TMJ should be checked and TMD should be treated to relieve the headaches and migraines.
Ear congestion
Due to the proximity of TMJ to the ears, it is very common for the ears to feel congestion, or to have ringing in the ears when the TMJ bones move or dislocate from their place. In this case, ENT's (ear doctors) won't find anything wrong with the ears, yet the patients keep complaining about their ears. Once the TMJ is put back into its natural position, the pressure put on the ears will be relieved and the congestion disappears.
Tingling or Numbness in the Fingers
When the TMJ is not in a balanced position, it affects the general posture of the body. When the posture is not straight and upright, the nerves coming out from the spine could be irritated, which could cause the numbness or tingling feeling in the fingertips.
Jaw Tracking
We use a state-of-the-art jaw tracking system that helps diagnose TMJ Dysfunction (TMD) by tracking the jaw movement. Research shows that there are certain jaw movements which show very specific types of TMJ dysfunction. For example, limited opening and closing or locking, jaw opening deviations and deflections, and restricted side-to-side jaw movements. All of these indications are widely accepted and published criteria for diagnosing TMD.
Joint Vibration Analysis (JVA)
The Joint Vibration Analysis (or JVA) has been accepted by the American Dental Association to help provide a fast, non-invasive method to accurately diagnose TMJ function and demonstrate the severity level of the problem.
Electromyographic Analysis (EMG)
We use an Electromyographic Analysis (or EMG) to measure muscle activity on head and neck muscles both at rest and in function. This is done by placing computerized sensors on the skin allowing us to accurately monitor muscle activity. Hyperactive muscles are common for patients experiencing pain symptoms associated with TMJ problems. Imbalances between right and left sides of the same sets of muscles are also typical. The EMG system is a safe and comfortable method do help detect such issues and getting to the root of a TMJ issue.
Neuromuscular TMJ Treatment
TMJ/TMD is treatable most of the time. Simple cases of TMJ can be treated with anti-inflammatory medications and a hot/moist compress.
Treatment for more complex cases usually consist of two phases:
Treatment of complex TMJ - Phase One:
Generally speaking, it includes the fabrication of an orthotic. An orthotic is an acrylic device that is worn on the lower teeth 24 hours a day. The orthotic is designed to reposition the jaw to the correct neuromuscular position. We analyze the bite, decide which muscles are causing the pain, and where the current position of the bone is and the disc. All this is done with the aid of advanced equipment like the TENS unit, K7 jaw tracking, Sonography, EMG's and advanced x-rays like Tomography, CT Scans and MRI's of the TMJ. This will help us determine the best and most comfortable position of the TMJ and the muscles. Once that position is determined, we place the orthotic on the lower teeth to keep the TMJ in that position. Orthotics usually are worn for 4-6 months or until most of the symptoms are relieved. Once an orthotic is in use, the symptoms start gradually disappearing until we reach a point that both the doctor and the patient are satisfied with. This concludes Phase I of the treatment.
Treatment of Complex TMJ - Phase Two:
After 4-6 months of relief and when the patient is no longer suffering from any TMD symptoms, Phase II will be considered. Phase II includes any of the following:
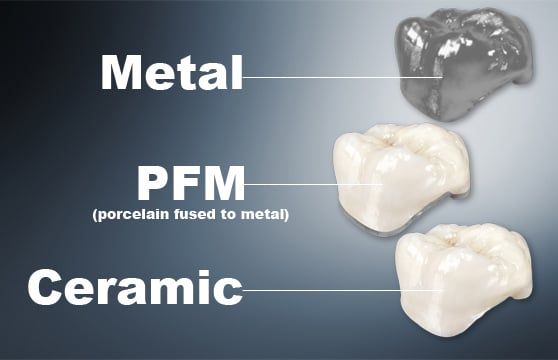
- Wearing a long term removable orthotic, full time or part time.
- Replace missing teeth.
- Orthodontic treatment (Braces).
- Restore all the lower and/or upper teeth with crowns and veneers to preserve the optimal occlusion (bite) that was achieved with the orthotic in phase I.
Most of the time, any of the above could be considered and chosen, depending on the patients' preferences and financial capability. If you are currently suffering from TMD, it is too early to think of phase II at this time, since it is important to get you out of your pain and symptoms.
Treating TMJ/TMD Caused by Dentures:
Many patients complain that when they received dentures, they noticed pain in the jaw, headaches, ear problems and other symptoms. Sometimes taking the dentures out will relieve those symptoms. If your dentures are not made to the correct bite, or vertical dimension, it will most likely cause these symptoms. Simple adjustments could get rid of these symptoms, but sometimes a whole new set of dentures need to be made according to the neuromuscular principles, to rid you of your headaches or jaw pain.
Orthotics or Bite Splints
An orthotic is an acrylic device that is worn on the lower teeth 24 hours a day. It is designed to reposition the jaw to the correct neuromuscular position.
An orthotic, sometimes called a Bite Splint, is a very effective method in relieving TMD symptoms. It provides an acrylic platform to bite against, sometimes moving the mandible to a new position that is more comfortable.
 Baby Bottle Tooth Decay
Baby Bottle Tooth Decay
 Baby Tooth Care
Baby Tooth Care
 Can you do all the work at once with a Sedation?
Can you do all the work at once with a Sedation?
Children Tooth Development
Early Childhood Caries
 Gaps between childs teeth
Gaps between childs teeth
 Having baby-teeth pulled
Having baby-teeth pulled
 How Enamel Fluorosis occurs
How Enamel Fluorosis occurs
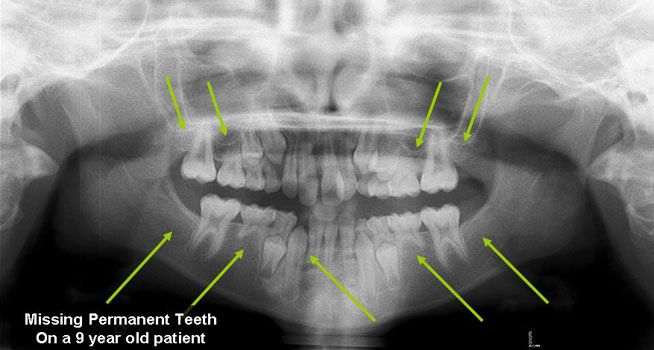 Missing Permanent Teeth
Missing Permanent Teeth
 My child has crooked teeth, will he or she need braces?
My child has crooked teeth, will he or she need braces?
 My child is getting shark teeth what can i do?
My child is getting shark teeth what can i do?
 My child's teeth have stains on them, are these cavities?
My child's teeth have stains on them, are these cavities?
 Pediatric Dental X-Rays
Pediatric Dental X-Rays
 Pediatric FAQs
Pediatric FAQs
 Thumb Sucking
Thumb Sucking
 Toothpaste for my child
Toothpaste for my child
 What is General Anesthesia and how safe is it?
What is General Anesthesia and how safe is it?
 What is oral sedation?
What is oral sedation?
 Will you need to give my child a shot to do the dental work?
Will you need to give my child a shot to do the dental work?